Sports and Musculoskeletal Injury
Our Sports and Musculoskeletal Injury Care focuses on precise diagnosis, advanced physiotherapy, and tailored rehabilitation to restore strength, flexibility, and performance. From acute sports injuries to chronic joint pain, our expert team ensures a safe, swift, and sustained recovery — helping you return stronger than before.
Advanced Physiotherapy & Rehabilitation
- Sports Injury Rehabilitation – Comprehensive recovery plans for ligament tears, sprains, muscle strains, and tendon injuries.
- Manual Therapy & Mobilization – Specialized hands-on techniques to relieve pain, restore joint mobility, and enhance muscle function.
- Post-Operative Rehabilitation – Targeted recovery programs following orthopaedic and arthroscopic surgeries for optimal function.
- Electrotherapy & Laser Therapy – Advanced modalities to reduce inflammation, promote healing, and relieve pain effectively.
- Kinesio Taping & Muscle Re-education – Supportive techniques to stabilize injured areas and prevent re-injury during activity.
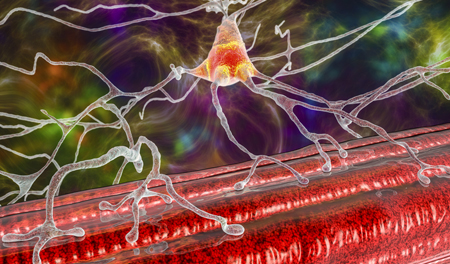
Symptoms & Causes
Common Symptoms:
- Joint pain, stiffness, or restricted range of motion
- Swelling, tenderness, or visible deformity around the injury site
- Muscle weakness or instability during movement
- Recurrent pain or discomfort during sports or daily activities
Common Causes:
- Overuse injuries from repetitive motion or training errors
- Improper warm-up or poor biomechanics during physical activity
- Sudden impact, falls, or collision during sports
- Weak muscles, tight ligaments, or previous untreated injuries
Prevention & Performance Care
- Warm up properly and stretch before and after physical activity
- Maintain good posture and use correct techniques during training
- Gradually increase exercise intensity to avoid overuse injuries
- Regular physiotherapy check-ups for injury prevention and performance optimization